Boosting vaccination: Accelerating vaccine uptake through communication science
by Victoria Ledford and Xiaoli Nan
Effective public health messages about vaccination can bolster human vaccine uptake to prevent the spread of infectious diseases. Despite this potentiality, the One Health framework that values an interdependent approach to health has not fully considered the role of communication science in promoting public health. In this article, we offer evidence-based recommendations for health practitioners and researchers creating vaccine promotion messages. An interdisciplinary field, communication science suggests that vaccine messages can change beliefs, attitudes, and behaviors through a systematic understanding of one’s audience and targeted and tailored health messages that appeal to beliefs about the outcomes of a behavior and beliefs about an individual’s behavioral efficacy. Implications for and challenges to vaccine communication are discussed.
Keywords: behavior change, Covid-19 vaccine, communication science, persuasion, public health.
Recognizing the interdependence of human, animal, and ecosystem health, the One Health framework calls for a transformative interdisciplinary approach that draws upon diverse disciplines. The One Health framework necessitates both a recognition of the connection between human, animal, and ecosystem health and an understanding that to tackle such issues, researchers must cross interdisciplinary bounds. The case of the Covid-19 pandemic offers a clear One Health challenge, as a disease originating in animals and transmitted to humans. While such zoonotic or vector-borne diseases (e.g., Covid-19, malaria) obviously benefit from an interdisciplinary One Health approach, the framework is much more far-reaching. Climate change, for example, also requires an understanding of human behavior, animal impact, and environmental changes – all elements that a One Health perspective considers. Despite the utility of a One Health approach, social sciences and, in particular, communication science have not played a central role in engaging One Health challenges (Lapinski et al., 2015). In this essay, we review evidence-based communication strategies that can be harnessed to accelerate human vaccine uptake and combat infectious disease outbreaks such as the ongoing Covid-19 pandemic.
As one of the most effective deterrents to infectious disease, vaccinations have curbed the spread of infectious disease in numerous instances: measles, various strains of hepatitis, smallpox, influenza, Human Papillomavirus, and most recently the novel coronavirus, or Covid-19. A One Health approach has been essential to all these efforts and remains essential to ongoing vaccine promotion efforts. Despite interdisciplinary and scientific advancements to produce vaccines, structural barriers to vaccination efforts persist, including but not limited to a lack of vaccination access, vaccine misinformation, and knowledge disparities. At the same time, human behavioral barriers may also deter vaccination efforts; negative and distrustful attitudes toward the Covid-19 vaccine are connected to less willingness to receive the vaccine (Paul et al., 2020). As health and science researchers process the vast communication landscape surrounding vaccines broadly and unique vaccines individually, we must continue to approach human vaccine uptake as a multi-faceted problem with multi-faceted solutions – a One Health perspective.
Communication science is an interdisciplinary field that has connections to persuasion and health message design and can offer solutions for public health messaging surrounding vaccines. Communication research fundamentally centers on the messages that influence beliefs, emotions, attitudes, and behavioral outcomes and as such offers theory and research that can help us understand how, why, and in what circumstances vaccine-related messages influence decision-making from a One Health perspective. Research has revealed the field’s potentiality for and effectiveness in changing health behaviors (Hornik, 2002). As human communication is only one element of the One Health approach, so too is the message only one part of the communication process. The communication process involves five key components: source (message sender), message (message content), channel (distribution means, e.g., in-person, social media), receiver, and destination (message effect) (McGuire, 1989). This article focuses on the message itself with reference to the other four parts when relevant.
Creating vaccine promotion messages
Communication science and its related subfield – health communication – offer theory-driven mechanisms for leveraging public health messaging to promote vaccine uptake. Together, communication science, health communication, and interdisciplinary research across the social sciences have been used to develop theories of behavior change that can direct the work of message creators. Central theories of behavior change still used to guide practice include the theory of reasoned action (Fishbein, 1979), the theory of planned behavior (Ajzen, 1991), social cognitive theory (Bandura, 2001), and the health belief model (Janz & Becker, 1984). Although each of these theories considers various concepts, the current essay focuses on insights related to their theoretical overlap.
These theories converge around three principles. First, there is a relationship between behavioral intentions and actual behavior. Although criticisms of this claim have been raised, this principle is affirmed by research studying the relationship between intention and behavior (O’Keefe, 2002). Second, self-efficacy, or beliefs that one can adequately perform a recommended behavior, is a central and consistent predictor of behavioral intentions (Sheeran et al., 2016). Finally, beliefs about the outcomes of a behavior (e.g., normative beliefs) influence behavioral intentions, with positive beliefs in favor of performing the behavior having a positive influence on intention.
Figure 1. Central behavioral elements that must be taken into account when developing messages to promote vaccines. / Source: Created by the authors from Fishbein & Capella (2006)
Behavioral Elements
|
Definition
|
Examples
|
| Action |
The decision-making required
|
Going to get vaccinated; making a vaccine appointment
|
| Target |
The object of decision-making
|
Receiving dose(s) of the vaccination
|
| Context |
Where the action takes place and under what circumstances
|
Taking 1–2 hours out of the day to go to the clinic and receive the vaccine
|
|
Time
|
When the action takes place
|
Getting vaccinated within the next 6 months
|
Before applying a model of behavior change to the creation of vaccine promotion messages, an important step is defining the scope of the advocated behavior. Not all behaviors require the same level of effort, consistency, or resources, nor do all behaviors activate the same set of beliefs. Therefore, health messages such as vaccine promotion messages should consider at minimum the action, the target, context, and time of an advocated health behavior (Fishbein & Capella, 2006). As the examples in Figure 1 illustrate, each of these behavioral elements requires consideration of a different message component. Communicating «go get vaccinated» does not provide the needed information to perform that action (i.e., a self-efficacy appeal), but instead only references the ultimate behavioral target. Importantly, additional factors such as structural barriers previously mentioned (e.g., vaccine access, resource disparities), cultural context, and other identity-based considerations should also be considered in tandem with these factors to truly promote effective targeted and tailored health messages.
Influencing outcome beliefs
Beliefs about the outcome of a behavior, are central to vaccine promotion messaging and to movement toward a One Health view. Outcome beliefs take various forms: utilitarian (costs or benefits such as physical harm or safety), social (rejection or approval), and value (confirming or contradicting one’s deeply held cultural, moral, or valued beliefs) outcomes (Bandura, 1998). Research surrounding each of these beliefs offers in-depth insights into a plethora of strategies to positively influence such beliefs. The current section offers a high-level overview of such strategies (see Nan et al., 2022).
Each type of outcome comes with a various set of expectations among the message receiver, and messages that match those expectations – or messages tailored to audience needs and beliefs – will be most effective. Message targeting and tailoring are related processes that involve designing a message for a particular group of people based on known characteristics or beliefs (targeting) and designing a message even more specifically based on an individual’s needs (tailoring). In the context of each set of outcomes (e.g., utilitarian, social, value), vaccine promotion messages will be most effective if these audience analysis tactics are taken into consideration.
Utilitarian outcomes that emphasize the health benefits of performing a behavior (e.g., getting an HPV vaccine) can be influenced by altering the focus of a message on either health promotion (i.e., acquisition of health benefits) or health prevention (i.e., avoidance of health risks). The decision to construct a message in promotion- or prevention-focus should be aligned with an audience’s orientation toward prevention or promotion messages. For example, people who are generally promotion-oriented are more likely to respond well to a vaccine message that states: «the HPV vaccination protects your long-term health», whereas people who are prevention-oriented will prefer messages that emphasize a prevention-focus, like «HPV vaccination can help you minimize your risk of cervical and other cancers». This strategy, known as regulatory fit (Higgins, 2000), is only one of many that can be used to craft public health messages around vaccination. Message designers can also emphasize other types of benefits for a health behavior, like those related to economic or global health concerns (e.g., «getting the Covid-19 vaccine will help bolster the economy»).
Social outcomes should also be centrally considered in the context of vaccinations. Research suggests that individuals make decisions based on their expectations about others’ behaviors (i.e., descriptive norms) and their perception of others’ approval of a particular behavior (i.e., injunctive norms). Appealing to these norms requires a message designer to understand the norm and, again, target a specific group. For example, messages motivating young adults to get vaccinated against Covid-19 may emphasize how common vaccination is among that age group (e.g., using a statistic) and share information on the social approval young adults express toward their peers who get vaccinated (e.g., «young adults are more likely to interact with and approve of their peers who have been vaccinated»).
Finally, value outcomes are often discussed colloquially but underexplored empirically. Value outcomes pertain to cultural beliefs or moral principles and may concern values such as collectivism or individualism, care or harm, liberty or oppression, etc. For example, Covid-19 messages that emphasize it is the «caring thing to do» or «collective good» to get vaccinated appeal to value outcomes. Although emphasizing values has the potential to positively affect behavior change, we are also keenly aware of how morality messages can create undue stigma toward those who do not perform the recommended behavior; such stigma can ultimately deter health efforts. Message designers should be cautious and avoid shame messages which could imply that inaction toward a behavior categorizes individuals into a group with a moral failing.
Influencing efficacy beliefs
How confident an individual feels in performing a recommended behavior is also a central determinant of behavior change. These beliefs concern various types of efficacy, including self-efficacy, or the belief that a person can perform the behavior; response efficacy related to the belief that carrying out the recommended behavior results in the expected outcome; and collective efficacy regarding a group’s self-efficacy beliefs. For vaccine communication, each of these types of efficacy remains increasingly relevant.
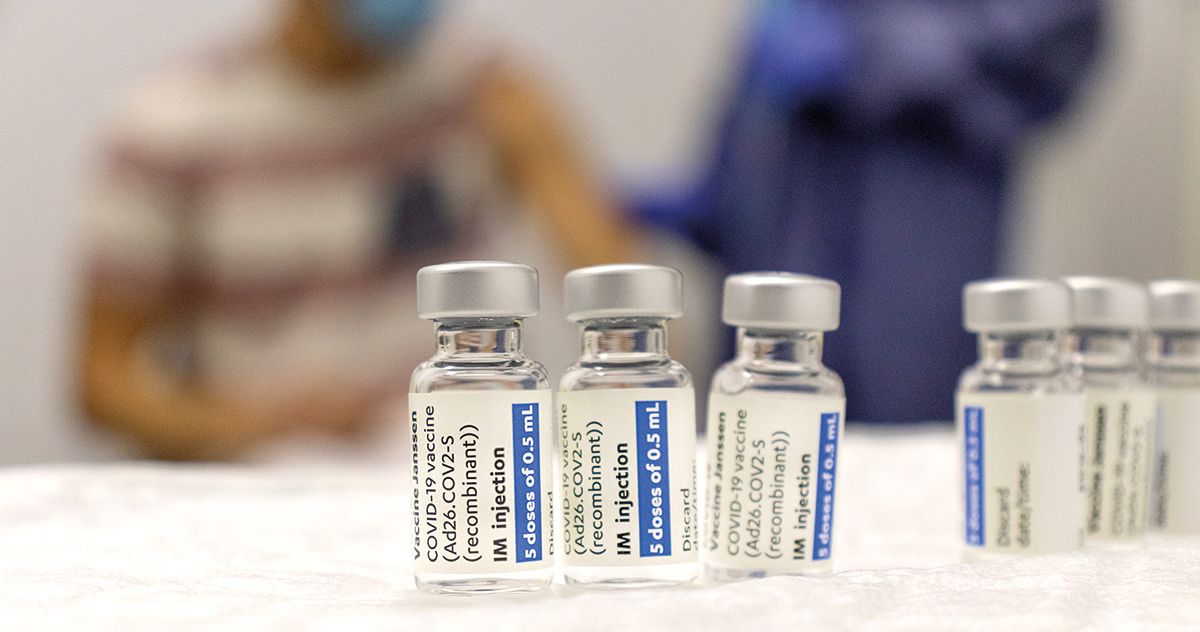
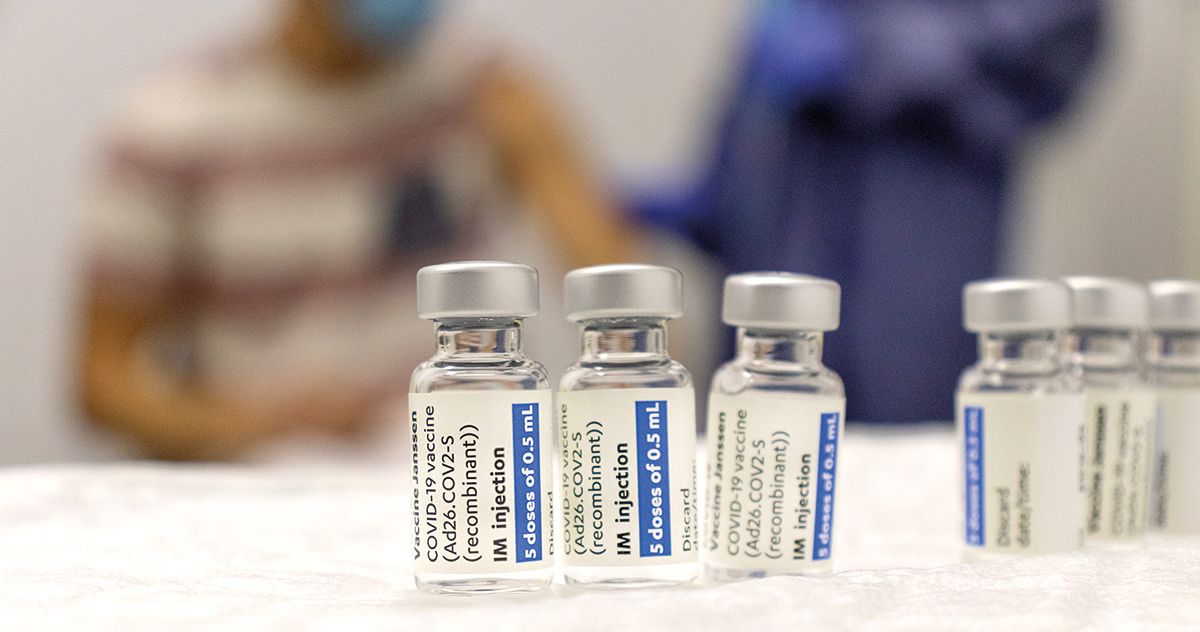
Covid-19 messages that emphasize it is the «caring thing to do» or «collective good» to get vaccinated can have a potentially positive effect on behavioural change, but can also create undue stigma toward those who do not perform the recommended behavior, which can ultimately deter health efforts. / Photo: Adrià Crehuet (Unsplash).
Communication research offers specific recommendations for bolstering an individual’s efficacy beliefs. These strategies include but are not limited to: (1) performance accomplishments that emphasize an individual’s previous success with performing the behavior, (2) vicarious experiences that depict similar models engaging in the recommended behavior with the desired outcomes, (3) verbal persuasion that relies on suggestion or a discussion of expectations for completing a behavior, and (4) emotional arousal that minimizes negative feelings toward a behavior (Bandura, 1977).
Vaccine messages attempting to increase self-efficacy, response efficacy, and collective efficacy may take different forms. For example, a person may not believe that they can go to the doctor’s office or clinic and get a shot within a particular time frame. Increasing self-efficacy in this situation could be done through any of the four above mechanisms. Using performance accomplishment as a strategy, a health communication message may emphasize an individual’s past vaccination success, whereas a message using vicarious experience might incorporate a visualization of a similar model or peer getting vaccinated (self-efficacy) and avoiding contracting the relevant health condition (response efficacy). The same type of logic can be applied for appeals to collective efficacy. Vaccination campaigns can rely on shared group characteristics to promote a collective belief in getting vaccinated (e.g., statewide vaccination efforts that appeal to citizenship and demonstrate the ease of getting vaccinated in a particular community or space).
Overcoming two key challenges
Promoting vaccination also requires an understanding of the challenges that may deter the effectiveness of communication campaigns. These challenges should be thought of not as deterrents, but rather as key considerations for health messengers. In approaching the design of vaccine promotion messages, an effective health campaign will first analyze its audience to determine what challenges may be present. Then, health communicators can use relevant theory to overcome such challenges.
Distrust
Health communication effectiveness is hampered by distrust of the message source. A key question long asked by communication scientists is: what is the role of message source in influencing perceptions of a message? Intuitive but perhaps underestimated, source trust can play a critical role in the health information landscape. Research has indicated that individuals may be more or less likely to trust various sources of health information, often preferring messages from in-groups, or communities in which the individual belongs, over outgroups (Hornsey et al., 2002). Social and demographic factors have also been found to affect trust perceptions of health information sources (Jackson et al., 2019). In cases of source distrust, messages may not even be received but instead may be considered overblown or disregarded altogether.
Source trust is an incredibly relevant consideration in the context of vaccination promotion. Childhood vaccination recommendations most prominently come from healthcare providers, and administration of vaccines in early childhood requires more contact with a healthcare provider. As individuals age, a series of more optional vaccines become available, e.g., HPV, influenza, meningitis, Covid-19. With age may come an increasing number of sources consulted regarding vaccines, or at times, a lack of source information. Adolescents, young adults, and parents may look to peers for vaccine recommendations, necessitating increased importance for ingroup health communication. Given the relevance of source trust, health message designers and practitioners should ensure they understand perceptions of trust in each community and encourage individuals to seek out trustworthy sources who have also developed strong audience relationships.
Misinformation and disinformation
With social media and the entrance to an age of infodemic, individuals must now navigate hordes of vaccine misinformation and disinformation. Each type of falsehood carries with it incorrect information, but important in the prefix is the intent behind information dissemination. Misinformation is false information spread without necessary malintent, whereas disinformation campaigns are intentionally used to spread false information and dissuade individuals from engaging in an action (e.g., getting vaccinated). Both types of false information have the potential to change outcome and efficacy beliefs and subsequently deter public health efforts. In the case of the Covid-19 pandemic, the mass circulation of myths about the vaccine led health experts and agencies to post debunking pages on websites dedicated to disproving common falsehoods.

Misinformation is false information spread without necessary malintent, whereas disinformation campaigns are intentionally used to spread false information and dissuade individuals from engaging in an action (e.g., getting vaccinated)./ Photo: Jordan Bracco (Unsplash)
Overcoming misinformation and disinformation is a critical area of communication science research with some key recommendations for vaccine communication. Researchers are currently examining the effectiveness of misinformation prevention – or «prebunking» (Lewandowsky & Van Der Linden, 2021). This strategy uses lessons from the well-tested inoculation theory (McGuire, 1961) to inoculate individuals against future intake of false information. Sharing the incorrect message an individual might receive along with a counterargument against that falsehood can equip people with information needed to refute the counterargument. These lessons can support vaccine communicators in being proactive against misinformation. For example, information shared about the rigor of the Covid-19 vaccine Emergency Use Authorization was an attempt to pre-bunk misinformation that the rate of vaccine development indicated a risky vaccine. Future vaccination campaigns should consider pre-bunking and inoculation strategies as direct methods to counter mis- and dis-information.
Forging a path forward
Scholars and practitioners across diverse fields should look to interdisciplinary insights, as championed by the One Health framework, that can guide vaccine promotion efforts and bolster public health. With theory-driven and empirically tested principles for promoting vaccination, communication science opens a door for public health messaging. Theory-driven message design requires a deep understanding of the audience for which a message will be delivered to. Scaffolded vaccination efforts at community, county, state, and nationwide levels are thus necessary to target and tailor effective health messages within groups. In creating these messages, designers should consider outcome beliefs, efficacy beliefs, and key challenges to vaccination efforts. By approaching vaccine promotion messages with a foundational understanding of the message and its influence on message recipients, health practitioners and scholars can continue the journey to bolster vaccine uptake. As the Covid-19 pandemic continues at the time of this essay’s publication, we cannot overstate the importance of effective and evidence-driven public health messaging as an integral component of the One Health endeavor.
References
Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179–211. https://doi.org/10.1016/0749-5978(91)90020-T
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191–215. https://doi.org/10.1037/0033-295X.84.2.191
Bandura, A. (1998). Health promotion from the perspective of social cognitive theory. Psychology and Health, 13(4), 623–649. https://doi.org/10.1080/08870449808407422
Bandura, A. (2001). Social cognitive theory: An agentic perspective. Annual Review of Psychology, 52(1), 1–26. https://doi.org/10.1146/annurev.psych.52.1.1
Fishbein, M. (1979). A theory of reasoned action: Some applications and implications. Nebraska Symposium on Motivation, 27, 65–116.
Fishbein, M., & Cappella, J. N. (2006). The role of theory in developing effective health communications. Journal of Communication, 56(s1), S1–S17. https://doi.org/10.1111/j.1460-2466.2006.00280.x
Higgins, E., T. (2000). Making a good decision: Value from fit. American Psychologist, 55(11), 1217–1230. https://doi.apa.org/doi/10.1037/0003-066X.55.11.1217
Hornik, R. (2002). Public health communication: Evidence for behavior change. Routledge.
Hornsey, M. J., Oppes, T., & Svensson, A. (2002). «It’s OK if we say it, but you can’t»: Responses to intergroup and intragroup criticism. European Journal of Social Psychology, 32(3), 293–307. https://doi.org/10.1002/ejsp.90
Jackson, D. N., Peterson, E., Blake, K. D., & Coa, K. (2019). American’s trust in health information sources: Trends and sociodemographic factors. American Journal of Health Promotion, 33(8), 1187–1193. https://doi.org/10.1177/0890117119861280
Janz, N. K., & Becker, M. H. (1984). The health belief model: A decade later. Health Education Quarterly, 11(1), 1–47. https://doi.org/10.1177/109019818401100101
Lapinski, M. K., Funk, J. A., & Moccia, L. T. (2015). Recommendations for the role of social science research in One Health. Social Science & Medicine, 129, 51–60. https://doi.org/10.1016/j.socscimed.2014.09.048
Lewandowsky, S., & Van Der Linden, S. (2021). Countering misinformation and fake news through inoculation and prebunking. European Review of Social Psychology, 32(2), 1–38. https://doi.org/10.1080/10463283.2021.1876983
McGuire, W. J. (1961). The effectiveness of supportive and refutational defenses in immunizing and restoring beliefs against persuasion. Sociometry, 24(2), 184–197. https://doi.org/10.2307/2786067
McGuire, W. J. (1989). Theoretical foundations of campaigns. In R. E. Rice & C. K. Atkin (Eds.), Public communication campaigns (Vol. 2, pp. 43–65). Sage.
Nan, X., Iles, I. A., Yang, B., & Ma, Z. (2022). Public health messaging during the Covid-19 pandemic and beyond: Lessons from communication science. Health Communication, 37(1), 1–19. https://doi.org/10.1080/10410236.2021.1994910
O’Keefe, D. J. (2002). Persuasion: Theory and research. Sage.
Paul, E., Steptoe, A., & Fancourt, D. (2020). Attitudes towards vaccines and intention to vaccinate against Covid-19: Implications for public health communications. The Lancet, 1, 100012. https://doi.org/10.1016/j.lanepe.2020.100012
Sheeran, P., Maki, A., Montanaro, E., Avishai-Yitshak, A., Bryan, A., Klein, W. M., Miles, E., & Rothman, A. J. (2016). The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: A meta-analysis. Health Psychology, 35(11), 1178–1188. https://psycnet.apa.org/doi/10.1037/hea0000387